In our inaugural year of 2019, LQN identified four program goals designed to address some of the most pressing health concerns as well as areas for the greatest cost savings within Medicaid:
Reduce inappropriate emergency department utilization
Promote evidence-based practice and reduce low-value care
2021-23 result:
Decrease in unnecessary lower back imaging
Decrease in unnecessary antibiotic Rx for sinusitis
LQN has subsequently identified four additional goals to address additional chronic healthcare challenges for the benefit of Louisiana’s Medicaid patients as well as the state’s population at large:
Improve breast cancer screening (2022-26)
Solution Preview
LQN is working to overcome the barriers to screening by expanding access to screening services, focusing on
MoreAutism and developmental screening in the first three years of life (2022-26)
Solution Preview
LQN is working to educate parents and caregivers along with primary care providers on the importance of early
MoreImprove prevention, screening, and treatment of childhood obesity (2023-27)
Solution Preview
Much of the initial work being carried out by LQN is to better understand how social determinants of health
More
Dr. Katie Queen is one of the few physicians in the country board certified in both Pediatrics and Obesity Medicine. By establishing the first Louisiana Childhood Obesity ECHO through LQN, she is able to extend her unique expertise to other clinicians across the state, caring for the most severe cases of pediatric obesity. Dr. Queen conducts live lectures and case consultations to expand treatment capacity throughout the state, including high-need rural communities.

Social determinants of health greatly impact Medicaid patients' well-being and the program's efficiency and cost. Factors such as income levels, education gaps, housing instability, food insecurity, and transportation barriers can worsen health disparities and raise chronic illness rates.
By establishing alternative resources, coordinating local support resources, and improving communication with the patient community, LQN hospitals are directing patients to more appropriate care, both improving outcomes and lowering Medicaid costs.
MORE
One solution to reduce hospital readmissions is to give patients the tools they need to follow their treatment plans and make it easier to access the medications prescribed to them. LQN has promoted the innovative “Meds to Beds” program throughout its member hospitals to ensure patients have all their medications prior to discharge. By reducing or eliminating all the extra steps a patient may need to take to access prescribed medicines, Meds to Beds improves adherence to their prescribed treatment and reduces the risk of medical complications, which may lead to readmission.
MORE
Dr. Jeffrey Elder smiled down at the treatment plan. He realized at that moment that LQN’s efforts to reduce Low Value Care had become ingrained in practices at University Medical Center New Orleans. He was huddling with physicians about how to treat a patient with chronic sinusitis, and the conversation followed LQN’s script to a tee. And it is a conversation happening at hospitals throughout Louisiana because of LQN, explained Dr. Elder.
MORE
Woman's Hospital in Baton Rouge, an LQN member, holds a remarkable distinction as the top deliverer of babies in the state. Renowned for its commitment to maternal and infant health, the hospital serves as a beacon of excellence, championing better outcomes for mothers and newborns. Through LQN, Woman's Hospital shares invaluable wisdom, guidance, and tools to aid fellow network members in implementing stronger protocols and enhancing care standards.
MORE
The MCIP program is available to all Medicaid Managed Care Organizations (MCOs) and Louisiana hospitals that are participating through two distinct networks. Louisiana Quality Network (LQN) is one of those networks.
The LQN banner represents a consortium of 12 healthcare systems and hospitals across Louisiana and five MCOs that came together to participate in the MCIP program. The Louisiana State University Health Sciences Center - New Orleans administers the program for the Network.
MORE
“A patient arrived at our Emergency Department with a headache and
high blood pressure just a week after giving birth. We followed
the protocols put in place through the MCIP program and discovered
a hemorrhage. Without these quality protocols, the new mom would
likely have been discharged without detecting the hemorrhage.
Because of the MCIP program, we prevented a possibly
life-threatening situation and avoided the need for a more costly
healthcare response.”
– Dr. Maria Buenaflor
Our Lady of the Angels Hospital, Bogalusa
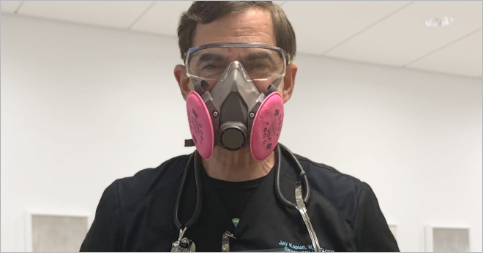
“On my last clinical shift, I explained to my patient that the CT
scan they were asking for would not give us the information we
needed and in addition would expose them to radiation the
equivalent of 100 chest x-rays all at one time. My patient very
much appreciated the explanation and our care. They went home more
knowledgeable about their illness and what to do in the future.
And we saved on the cost of the test, which would have been well
over $1,000.”
- Jay Kaplan, M.D., FACEP
Medical
Director of Care Transformation, LCMC Health

“Patients are often confused, anxious, and overwhelmed after
discharge from the Emergency Department. Aligned with the goals of
the MCIP program, we’re helping patients navigate the complicated
healthcare system, arming them with the knowledge they need to
manage their follow-up instructions safely at home and help ease
their concerns. This helps patients connect to the most
appropriate point of care and allows our Emergency Departments to
focus on the patients most in need.”
– Lisa McGowan, RN
LCMC Care Manager

In Tangipahoa Parish, LQN member North Oaks Health System is already seeing a reduction in avoidable healthcare services. Aligned with the MCIP program, the hospital is taking proactive steps to help patients, like Mr. Abbott, stay healthy. They call to check on him, to make sure he’s taking his medication, and to remind him about upcoming appointments. They’re also quarterbacking his team of care providers to improve efficiencies and outcomes, and they even arrange transportation to ensure Mr. Abbott can make it to treatments.

In Baton Rouge, LQN member Our Lady of the Lake Regional Medical Center created a “Navigation Program” in the Emergency Department. Diane Reidy, the Senior Director for Care Management, explains that people who lack financial resources or insurance traditionally have used ERs as their primary healthcare resources, because they knew they were places where they could get care. She’s quick to point out that many such patients were financially stable until a major accident or illness wiped out their finances.
MORESend us a message if you’d like additional information on LQN